Clinical Characteristics and Therapeutic Advances inFunctional Dyspepsia Combined with Gastroesophageal Reflux Disease (Part 1)
Introduction
Functional dyspepsia(FD) and gastroesophageal refluxdisease(GERD), which are among the most prevalentupper gastrointestinal(Gl) disorders, respectivelyrepresents the most common type of functionalgastrointestinal disorders (FGIDs) and acid-relatedmotility disorders. These two conditions often coexist,forming an "overlap syndrome".' Epidemiologicaldata indicate that the co-occurrence of these twoconditions far exceeds random probability, suggestinga shared pathophysiological basis, such as thegeneralization of visceral hypersensitivity, gastric andduodenal dysmotility, and the dysregulated brain-gutaxis. (1-3'This overlap is not merely a simple addition ofsymptoms but may form a unique "overlap syndrome"with distinct characteristics, leading to more complexsymptoms in patients (such as the co-existence ofepigastric pain, postprandial fullness, and reflux andheartbur), more severe impairment of quality of life,and poor response to traditional monotherapy strategiestargeting either FD or GERD. At present, although theRome IV diagnostic criteria provide a framework forthe diagnosis of comorbidity of these two conditions,4 there is still a lack of systematic consensus ontheir intrinsic connections and optimal managementpathways in clinical practice. Therefore, this reviewaims to summarize the latest research progress onthe comorbidity of FD and GERD, explore symptomcharacteristics, pathophysiological mechanisms,and evidence-based integrated treatment principles.Therefore, it may provide an overview for diagnosticand therapeutic approaches for clinical practice andimprovement of patient prognosis.
1.FD
FD is a one of the most common FGIDs, namelydisorders of gut-brain interaction (DGBD). Accordingto the Rome IV criteria, it is defined as persistent orrecurrent epigastric pain or burning, postprandialfullness, or early satiation, in the absence of anystructural or metabolic diseases that would likelyexplain the symptoms.'4 Epidemiological studies have shown that the prevalence of FD in the generalpopulation worldwide is about 7%-30%, and itaccounts for more than 40% of medical visits togastroenterology outpatient clinics, thus constituting asubstantial medicare burden, (5-8)
1.1 Pathophysiology of FDThe pathophysiological mechanisms of FD arecomplex and involve interactions among multiplefactors at the brain-gut axis level, mainly including thefollowing aspects:
1) Gastric and duodenal dysmotility. Approximately30% of patients with FD experience delayed gastricemptying, which is associated with symptoms suchas nausea and vomiting. Impaired gastric receptiverelaxation is an important mechanism underlyingpostprandial fullness and early satiation.
2) Visceral hypersensitivity. Patients have a lowerperception threshold and increased responsivenessto physiological or noxious stimuli such as gastricdistension and chemical irritation. This is one ofthe core mechanisms underlying epigastric pain anddiscomfort in FD.
3) Impaired mucosal integrity and low-gradeinflammation: Recent studies have shown that somepatients with FD enhibit impaired barrier function ofthe duodenal mucosa, increased infiltration of immunecells (such as eosinophils and mast cells), and low-grade mucosal inflammation, as well as intestinaldysbiosis. These alterations may directly activate localnerve endings and contribute to the development of FDsymptoms.
4) Central mechanisms. Psychosocial factors such asanxiety and depression, as well as psychological stress,can affect Gl sensory and motor functions via thebrain-gut axis. These factors are important triggers forthe exacerbation and chronicity of FD symptoms. 9.10]
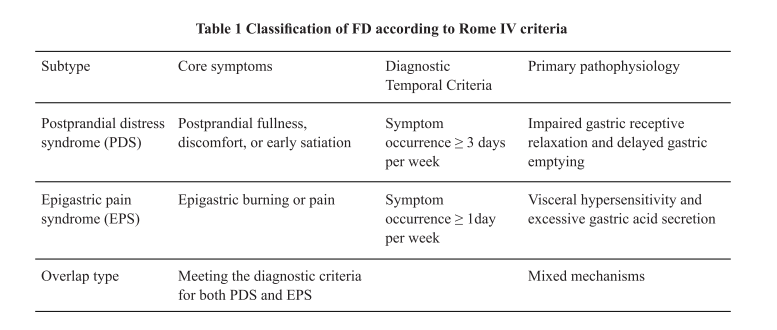
1.2 Classification of FDBased on the predominant symptom pattern, the RomeIV criteria divide FD into two subtypes, which oftenoverlap (Table 1). [14]
2.GERD
GERD is an upper GI disorder characterized by theabnormal reflux of gastric and duodenal contents intothe esophagus, causing symptoms such as heartburnand regurgitation or leading to complications. It isprimarily classified into erosive esophagitis (EE), inwhich mucosal breaks are observed on endoscopy, andnon-erosive reflux disease (NERD)with the mucosaremaining intact. The core pathogenesis of GERDinvolves the imbalance between the anti-reflux defensemechanisms (such as lower esophageal sphincterfunction and esophageal clearance capacity) and theinjurious effects of the refluxed agents (such as gastricacid and pepsin). Other factors, including increasedesophageal sensitivity and delayed gastric emptying,also play a role. The diagnosis of GERD integratessymptoms and objective evidence. Typical symptomsinclude heartburn and regurgitation. The presence ofesophagitis on endoscopy (especially Los Angelesgrade B or above) is an important objective evidence.The gold standard for diagnosis of GERD is 24-houresophageal impedance-pH monitoring, which showsesophageal acid exposure time >6%. A significantcorrelation between reflux events and symptom onset(symptom association probability>95%)serves as supportive evidence. Notably, objective physicalexaminations (such as endoscopy and 24-houresophageal impedance-pH monitoring) are crucial forconfirming the diagnosis, classifying the disease, andguiding the management of refractory cases, [11,12]
3. The Rome IV criteria for the classification of FD in the context of coexisting upper Gl symptoms
The core of the Rome I'V diagnostic system is a"positive diagnosis" based on symptom clusters, andit allows for multiple diagnoses to be made if each setof diagnostic criteria is met. This principle provides aclear framework for understanding the overlap betweenFD and GERD.
3.1 Diagnosis and differential diagnosis of FDIt is essential for the diagnosis of FD that the symptomcriteria should be met (Table 1). In clinical practice,it is essential to be vigilant and screen for "alarmsigns," such as unexplained weight loss, progressivedysphagia, recurrent vomiting, and GI bleeding. Forpatients with alarm signs or older age (typically>50-60years) presenting with new symptoms, a gastroscopyis recommended to rule out organic diseases such as peptic ulcer disease and gastric cancer. For youngerpatients without alarm signs, empirical treatment maybe considered initially, with endoscopy performed ifthe treatment is ineffective. [4]
3.2 The taxonomic concept of' overlap between FD and GERD
When a patient displays both epigastric symptoms andsymptoms of reflux/heartburn, the Rome IV criteriaencourage physicians to conduct the following separateassessments:
1) Diagnosis of FD.
2) Diagnosis of GERD. Diagnosis criteria for FD andGERD have been described above.
3) Diagnosis of functional heartburn. Patients withfunctional heartburn exhibit obvious heartburnsymptoms. However, their esophageal mucosa appearsnormal on endoscopy, and 24-hour esophageal pH-impedance monitoring suggests that symptom onset isnot temporally related to reflux events.
4) Diagnosis of reflux hypersensitivity. Patients withreflux hypersensitivity display symptoms of heartburnor chest pain, with normal esophageal mucosa onendoscopy. However, physiological reflux (acidic ornon-acidic) is sufficient to trigger symptoms of patientswith reflux hypersensitivity, indicating a clear temporalrelationship between reflux events and symptom onset.These properties suggest the presence of esophagealvisceral hypersensitivity. [4.13.14]
Therefore, the "reflux-like symptoms" associated withFD may arise from the following three scenarios:
1) Real GERD(excess acid reflux).
2)Functional heartburn (unrelated to reflux).
3) Reflux hypersensitivity (exaggerated response tophysiological reflux). The latter two are categorizedas functional esophageal disorders, and their treatmentstrategies differ from that of GERD. Notably, accuratedifferentiation is crucial for selection of precisetreatment approaches for patients with both epigastricsymptoms and symptoms of reflux/heartburn.
References
1. Geeraerts A, Van Houtte B, Clevers E, Geysen H,Vanuytsel T, Tack J, Pauwels A. Gastroesophagealreflux disease-functional dyspepsia overlap:Do birds of a feather flock together? Am JGastroenterol.2020;115(8):1167-1182.
2. Gwee KA, Lee YY, Suzuki H, Ghoshal UC, HoltmannG, Bai T, Barbara G, Chen MH, Chua ASB, GibsonPR, Hou X, Liu J, Nakajima A, Pratap N, SachdevaS, Siah KTH, Soh AYS, Sugano K, Tack J, TanVPY, Tang X, Walker M, Wu DC, Xiao YL,ZulkitiKK, Toh C. Asia-Pacific guidelines for managingfunctional dyspepsia overlapping with othergastrointestinal symptoms. J Gastroenterol Hepatol.2023;38(2):197-209.
3. Ohara S, Kawano T, Kusano M, Kouzu T. Surveyon the prevalence of GERD and FD based on theMontreal definition and the Rome IIl criteria amongpatients presenting with epigastric symptoms inJapan.JGastroenterol.2011;46(5):603-611.4. Drossman DA. Functional gastrointestinal disorders:history, pathophysiology, clinical features and RomeIV. Gastroenterology.2016:S0016-5085(16)00223-7.
4. Drossman DA. Functional gastrointestinal disorders:history, pathophysiology, clinical features and RomeIV. Gastroenterology.2016:S0016-5085(16)00223-7.
5. Tack J, Palsson OS, Bangdiwala SI, Schol J, CarboneF, Van Den Houte K, Broeders B, Drossman D,Dumitrascu DL, Fang X, Fukudo S, GhoshalUC, Kellow J, Khatun R, Okeke E, QuigleyEM, Schmulson M, Simren M, Whitehead WE,Whorwell P, Sperber AD. Functional dyspepsia andits subgroups: prevalence and impact in the RomeIV global epidemiology study. Aliment PharmacolTher.2025;62(3):330-339.
6. Lee K, Kwon CI, Yeniova AO, Koyanagi A, JacobL, Smith L, Lee SW, Rahmati M, Shin JY, Shin JIl,Cho W, Yon DK. Global prevalence of functionaldyspepsia according to Rome criteria, 1990-2020: asystematic review and meta-analysis. Sci Rep. 2024Feb20;14(1):4172.
7. Kim SE, Kim N, Lee JY, Park KS, Shin JE, NamK, Kim HJ, Song HJ, Joo YE, Myung DS, SeoJH, Jo HI, Kim SM, Lim SH, Kim HI, Baik GH,Choi SH, Choi SC. Prevalence and risk factors offunctional dyspepsia in health check-up population:A nationwide multicenter prospective study. INeurogastroenterol Motil.2018;24(4):603-613.
8.Quach DT, Ha QV, Nguyen CT, Le QD,Nguyen DT, Vu NT, Dang NL, Le NQ.Overlap of gastroesophageal reflux diseaseand functional dyspepsia and yield ofesophagogastroduodenoscopy in patientsclinically fulfilling the rome IV criteria forfunctional dyspepsia. Front Med (Lausanne).2022;9:910929.
9. Ford AC, Mahadeva S, Carbone MF, LacyBE, Talley NJ. Functional dyspepsia. Lancet.2020;396(10263):1689-1702.
10.Wauters L, Talley NJ, Walker MM, Tack J, VanuytselT. Novel concepts in the pathophysiologyand treatment of functional dyspepsia. Gut.2020;69(3):591-600.
11.Patel J, Wong N, Mehta K, Patel A. GastroesophagealReflux Disease. Prim Care.2023;50(3):339-350.
12.Roark R, Sydor M, Chatila AT, Umar S, Guerra R,Bilal M, Guturu P. Management of gastroesophagealreflux disease. Dis Mon.2020;66(1):100849.
13.Rengarajan A, Pomarat M, Zerbib F, GyawaliCP. Overlap of functional heartburn and refluxhypersensitivity with proven gastroesophagealreflux disease. Neurogastroenterol Motil.2021;33(6):e14056.
14.Sawada A, Sifrim D, Fujiwara Y. Esophageal RefluxHypersensitivity: A Comprehensive Review. GutLiver.2023;17(6):831-842.

